Introduction
Worldwide, it is estimated that there are 40 million infected persons with HIV / AIDS. The incidence during pregnancy varies from 0.3 to 2%. Mother to child transmission accounts for most HIV infections among children. Though plasma viral HIV – 1 RNA levels have proven to be the best predictor of risk of transmission and other complications, CD4 count also may have a predictive role. This study summarizes the implications of CD4 count in perinatal outcome in our institution.
Aims and Objectives:
Our aim is to correlate the maternal CD4 count to the perinatal outcome.
Study Design:
A prospective ongoing study is being conducted including all seropositive HIV women admitted to the Institute of Maternal and Child Health,Calicut, Kerala from January 2005 till date. A total of 69 cases were analyzed and the perinatal outcome studied in terms of preterm rates, birth weights, perinatal morbidity, perinatal mortality and vertical transmission. The data will be analysed using Chi square and Spearman’s correlation studies.
Results and conclusion:
Total numbers of 69cases were followed up for a period of 18 months and statistically significant results with Chi square and Spearman’s correlation could be established with:
- Vertical transmission and maternal CD4 count (p value <0.0001)
- Lack of antiretroviral treatment and vertical transmission (p value = 0.049)
No significant correlation could be established between maternal CD4 count and preterm delivery, birth weight, perinatal morbidity and mortality.
Key words: Maternal CD4 count, Perinatal outcome
Introduction
Modern medicine has made life colourful, but the happy scenario was rudely shattered in early 80’s with the advent of a new virus, later identified as the HIV virus. From an exclusively male disease HIV / AIDS is rapidly becoming equally distributed in both sex – feminization of the epidemic. Innocent childhood is also getting nipped in the bud.
HIV transmission in India
74-82% through heterosexual route, 7.4% homosexual, 4-7% blood transfusion, 4-8% intravenous drug users and perinatal route only 1.5%. But the chances of acquiring HIV following a single exposure is 0.1 to 2% by heterosexual route, 90% by blood transfusion and a glaring 30% by perinatal transmission. In India were there are around 29 million deliveries per year, if the prevalence rate is taken as <1%, around one lakh HIV positive mothers deliver every year. If MTCT is taken as 30% – 30,000 infants will be affected per year – if no preventive measures are taken. About 40% of the women who are of childbearing age do not know that perinatal transmission of HIV is preventable. The appropriate and timely intervention can slash the rates to <2%.
The relevance of CD4 cells
The CD4 + T cells are the main targets of HIV and the progressive destruction of these cells is characteristic of all stages of HIV disease. The CD4 + T cells serve as surrogate markers to monitor the progression of HIV infection. These cells are destroyed by two mechanisms mainly direct damage by the virus and the immune mechanisms triggered during the course of HIV infection.
Mechanism and timing of transmission
Risk factors of MTCT of HIV
Antepartum factors: High maternal viral load, low maternal CD4 count, rapid progression to AIDS, vitamin A deficiency, illicit drug use, amniocentesis in third trimester, lack of antenatal care.
Intrapartum factors: Cervical vaginal HIV levels, mode of delivery, prolonged rupture of membranes, premature delivery, invasive fetal monitoring and instrumental deliveries.
Postpartum factor: Breast feeding
Maternal plasma viral load is recognized as a strongest predictor of transmission, unfortunately viral load testing is not freely available nor feasible, especially in developing countries like India, where the role of maternal CD4 count in prediction of MTCT requires serious consideration. The aim of this study was to correlate the maternal CD4 count to the perinatal outcome. Outcome in terms of vertical transmission, intrauterine growth restriction, preterm births, perinatal mortality and morbidity.
Methods
Women attending in Antenatal Clinic of our PPTCT centre from January 2005 were counseled regarding the HIV infection with special reference to the possibility of HIV transmission from their parents to their children. After an informed consent and pretest counseling, HIV status with rapid testing methods was done and post test counseling was also given. The importance of antiretroviral therapy was stressed to the patients who were found to be sero positive and CD4 counts were analysed. ART was started for all those patients who opted to continue their pregnancy. All seropositive women admitted to our institute at the onset of labour were given oral nevirapine according to NACO guidelines. Labour was conducted strictly adopting universal precautions, babies were all given nevirapine syrup. All mothers were counseled about the merits and demerits of breast feeding. Mothers and babies were followed up till 18 months of age and the babies were tested for HIV infection at 18 months with ELISA, under assumption that a positive antibody test at 18 months of age indicated that the baby was infected. We extracted the data from medical records without taking the identity of women into account and analyzed the data for study purpose and followed up the patients upto 18 months.
Result
The total number of deliveries from the period of Jan 2005 to September 2011 were 121040. Total number of seropositive women were 69. The prevalence in our population was found to be 0.057%.
Mode of delivery (Table 1)
Out of the 69 cases followed up 13 (18.8%) underwent vaginal delivery and 56 (81.2%) underwent LSCS. Out of the positive babies 40% were born abdominally and 60% vaginaly.
Breast feeding (Table 2)
Only two babies (2.85%) were breast fed ;58 (97.15%) opted for formula feeds.
Vertical transmission (Table 3)
The vertical transmission rate in our population was found to be 7.2%. 72.5% of the babies were negative at the end of 18 months. There were Two defaulters in the study population.Twelve babies are yet to complete the 18 months follow up ELISA.
Antenatal ART
61 women (88.4%) had taken antenatal ART. 8 women (11.6%) did not receive ART. Among the positive babies, it was found that 60% of mothers did not receive ART.
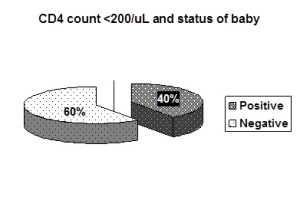
CD4 count (Table 4 & Fig. 1))
10 women (14.5%) had a CD4 count of <200. 12(17.4%) women had a CD4 count of200-350and 47(68%) had a count>350 and it was found that 40% of women with CD4 count <200 had passed on the dreaded infection to the children.
Discussion
The prevalence of HIV positive women in our population is 0.057%.
The present study depicted that a strikingly large number of women belonged to 26-34 years age group (63.8%), the productive age group. < 25 years contributed to 30.4% of cases and >35 years 5.8%. It was found that the majority of the women in our study by detected to be positive in the second trimester (55.1%) and 40.6% were detected only in third trimester, thus highlighting the importance of early antenatal screening.
88.4% (61 cases) received antiretroviral therapy. Retrospective analysis showed that 60% of the women in our study whose children were diagnosed to be positive had not take ART (p value 0.049). This fact highlights the need to be more vigilant to councel the expected mothers and to uphold there confidence regarding the need, safety and efficacy of antiretroviral treatment. Regarding the mode of delivery 55 cases (81.2%) of our cases underwent elective LSCS and around 13 cases (18.8%) had vaginal delivery. Evidence shows that performing a cesarean section prior to the onset of labour can reduce the risk of infection upto 4 fold because it minimizes the exposure of the child to maternal body fluids. It was noted from our study that among the positive babies ,60% were delivered vaginally and 40% delivered by LSCS and it was also noted that there was no increased morbidity in the HIV positive women undergoing LSCS in comparison to the normal control group.
Interestingly, in our study majority of the babies who eventually turned out to be positive were males. Similar observations were mentioned in a few studies but the scientific basis is yet to be established.
Though intrauterine growth restriction has been mentioned as one of the perinatal complications, it was noted in our study that 69% of babies had birth weight above 2.5kg. So we could not establish a significant corelation of growth retardation and maternal hiv infection.
All our patients except two preferred formula feeds. 97.15% of our babies were formula fed.
Going into the core of our study we could establish that the vertical transmission rate after a follow up of 18 months in our population turned was 7.2%. We had two defaulters (2.9%) ,72.5% of our babies turned out to be negative and 12(17.4%) remains pending at the end of 18 months ELISA.
The CD4 count was the most important variable in our study; we had 10 cases (14.5%) with CD4 count <200/mL and 59cases (85.5%) with CD4 count >200/mL. Quite interestingly 80%the mothers whose babies eventually turned out to be positive had a CD4 count <200/mL and 40 % of the women with CD4 count <200 transmitted the disease to her child. A significant correlation could be established between the maternal CD4 count and vertical transmission with a p value of <0.0001. Spearman’s correlation was also found to be significant.
All the 5 positive babies turned up with morbidities like severe lower respiratory tract infection, anemia and associated morbidities. From our study we could establish no correlation between CD4 count of the mother and perinatal mortality or preterm deliveries.
Finally we would like to highlight the importance of primary prevention and councelling. Motivation for universal voluntary screening can be a stepping stone to a better future. Proper health education regarding HIV / AIDS and ART may alleviate the social stigma and motivate towards the adherence to ART wen needed and would definitely be much better in the subsequent years. The need for antepartum, intrapartum and postpartum precaution deserves a special mention.
Conclusion
- The vertical transmission rate in our study population was 7.2%
- 80% the babies who proved positive had a maternal CD4 count <200/mL (p value <0.0001)
- Majority of mothers of seropositive babies had not received ART (60%, p value = 0.049)
- Women screened positive late in pregnancy had the positive babies probably because of lack of timely intervention
- Although majority of the HIV exposed babies were females, 80% of the affected children were males.
- Babies born vaginally were more at risk.
- No significant correlation could be established between low maternal CD4 count to birth weight, preterm delivery, and perinatal mortality.
Acknowledgement
We thank all members of our department and the PPTCT team for their support and encouragement. We appreciate all the help lend to us by our library and statistical department.
References
- Newell ML, Dunn DT, Peckam CS, et al. Vertical transmission of HIV -1: Maternal immune status and obstetric factors. The European Collaborative study.
- Management of HIV positive pregnancy. www. info. gov. hk/aids/pef/g190htm/35.htm
- Prevention of parent to child transmission of HIV – scenario of West Bengal. J Obstet Gynecol India, vol. 58, No.3: May/June 2008
- Leroy et al,AIDS 2005, vol 19(16);1865-75(17)
5. Shaffer N et al. Lancet 1999 March6; 353:773-80(14)
6. Humphery j etal. Personal communication 2010
7. Mayaux M J JAIDS 1995 Feb1;8:188-94(18)
8. Working paper on Mother-to-child HIV transmission rates for use in spectrum;6 june 2011 UNAIDS reference group on estimates, modeling and projections.
Table 1 : Mode of Delivery
No. of cases Percentage
Vaginal 13 18.8%
LSCS 56 81.2%
Total 69 100%
Table 2 : Breast Feeding
No. of cases Percentage
Breast fed 2 2.90%
Not breast fed 67 97.10%
Total 69 100%
Table 3 : Vertical transmission
No. of cases Percentage
Positive 5 7.2%
Negative 50 72.5%
Defaulters 2 2.9%
Table 4 : CD4 count
No. of cases Percentage
<200/mL 10 14.5%
200-350/mL 12 17.4%%
>350/mL 47 68%
Figure-1
About the Authors:
Guhan Beena, Associate Professor1
Rajmohan Laxmy, Postgraduate Student1
1Department of Obstetrics and Gynecology
Institute of Maternal and Child Health
Medical College,
Calicut, Kerala.
Address for correspondence:
DR. BEENA GUHAN
HOUSE NO. 33/5589B
SUBSTATION ROAD
CHEVAYURPO
CALICUT
KERALA – 673 017
Tel: 9446046444
E-mail: beenaguhan@gmail.com